Win this $3.6 MILLION Gold Coast Prize Package!
WIN this Burleigh Beauty!
Now THIS is the place to be!
Home to some of the best beaches in Australia, Burleigh is the sparkling jewel in the Gold Coast crown and is the location of Mater Prize Home lottery No. 312.
Just minutes from stunning Burleigh Beach is this sprawling, fully furnished 4-bedroom property. WIN and you could be living the mortgage-free life in this unrivalled location. PLUS, enjoy the coastal lifestyle with a Land Rover Defender 110 D300 SE, PLUS a Sea-Doo GTR230 and trailer, PLUS two McTavish Noserider surfboards and accessories, PLUS $50K in gold bullion!
This incredible $3,678,618 Gold Coast prize package could be all yours for just $2!
Download Mater Prize Home lottery No. 312 brochure
30 Banksia Broadway , Burleigh Waters, QLD, 4220
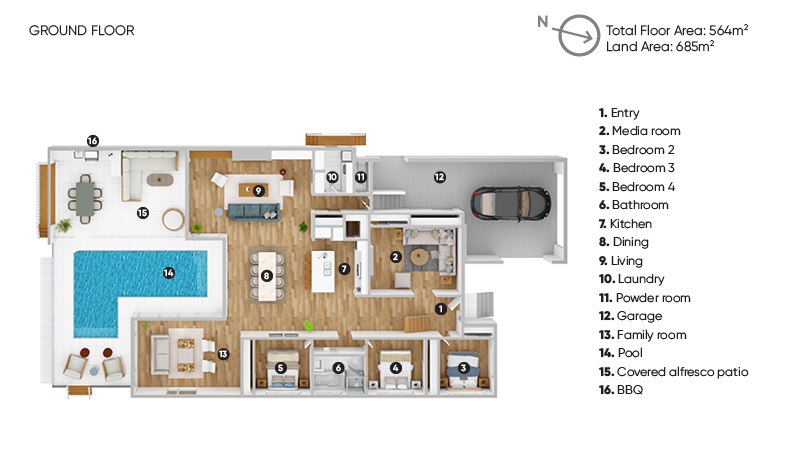
Floor Plan
Take a tour
The place to be...
Characterised by its world-class surf breaks, gorgeous beaches, scenic nature walks, and a lively café and dining scene, it’s no wonder Burleigh is a much sought-after location.
This Mater Prize Home is centrally located to all the best things the region has to offer, with Burleigh Heads beach 3 minutes from home and Surfers Paradise 24 minutes. The vibrant James Street is only 5 minutes down the road and boasts some of the best cafés, restaurants and boutiques on the Gold Coast.
Investment report

Rental potential
$91,000 p/y *(Furnished)*Based on estimated rental return Dec 2023
Market value
$3,275,000 **Based on current market value Dec 2023Visit the home
30 Banksia Broadway Burleigh Waters, QLD, 4220The prize home will be open 9am to 5pm daily, from Wednesday 7 February to Saturday 20 April 2024. The home will be closed on Good Friday (29 March). We look forward to welcoming you to this beautiful Burleigh home!